In a significant medical engineering achievement with broad implications for critical care, a surgical team at Northwestern University successfully kept a patient alive for two days using a bespoke artificial lung system following the removal of severely damaged organs. The procedure, detailed in the journal Med, establishes a crucial precedent: a true artificial lung can maintain systemic viability until a donor organ becomes available.
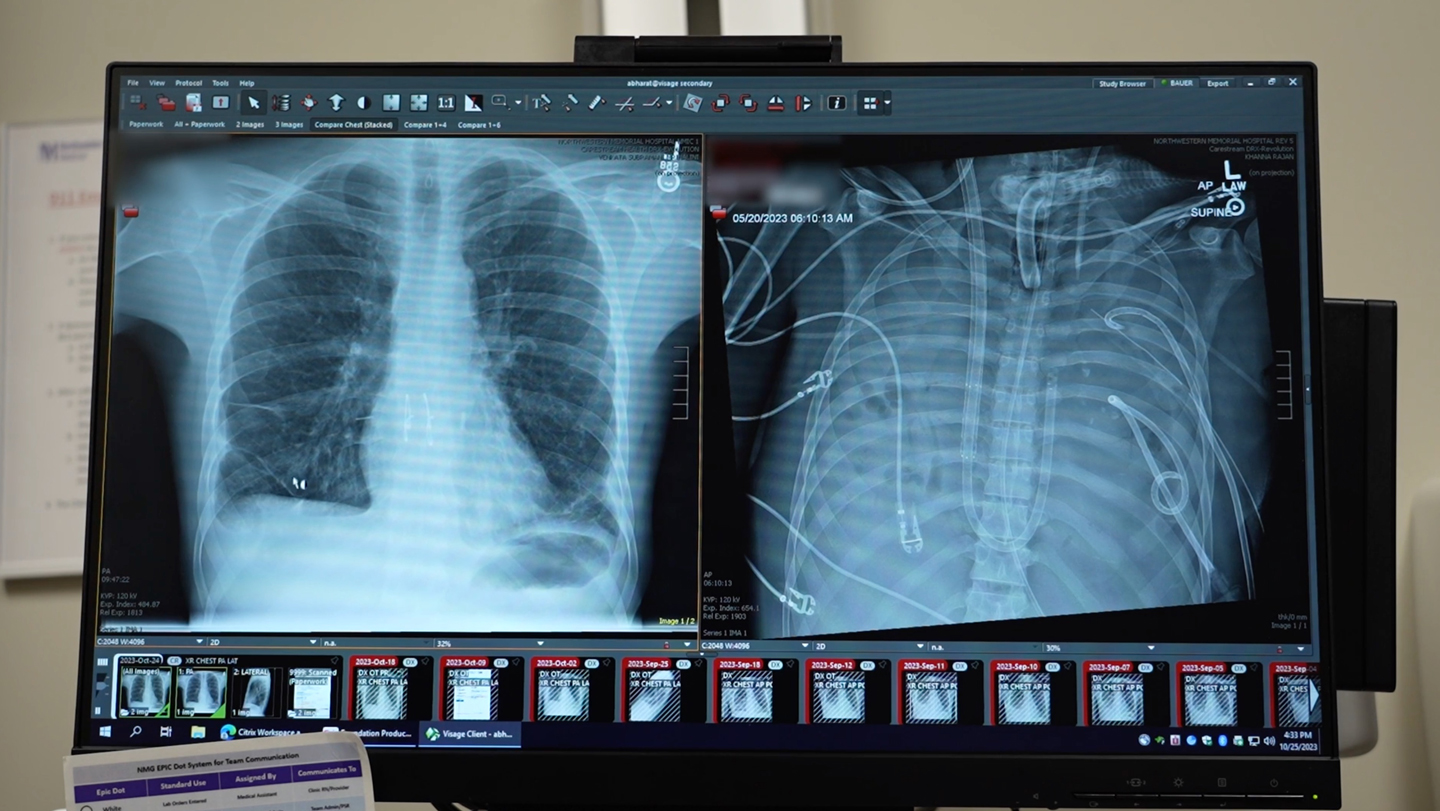
The case involved a 33-year-old man who suffered catastrophic lung failure due to a severe influenza B infection compounded by a subsequent, antibiotic-resistant Pseudomonas aeruginosa bacterial infection. Dr. Ankit Bharat, chief of thoracic surgery at Northwestern, noted the patient was “actively dying,” with molecular tests indicating no possibility of natural recovery. Standard transplant protocols were complicated by the active infection, necessitating the radical step of removing the diseased lungs entirely.
The custom-designed artificial lung system functions by diverting blood from the right side of the heart, artificially performing gas exchange—oxygenating the blood and removing carbon dioxide—and then returning the vitalized blood to the left side of the heart for systemic circulation. Crucially, unlike conventional Extracorporeal Membrane Oxygenation (ECMO), this configuration provides necessary support for the heart’s pumping action, effectively mimicking the complete physiological role of the native lungs.
While ECMO has previously served as a temporary measure, it lacks the comprehensive circulatory support provided by this new device. Researchers had prepared for a potentially lengthy sustainment period, anticipating weeks for the systemic infection to clear sufficiently to permit a transplant.
However, the removal of the infected lungs—the primary source of the bacterial load—precipitated a rapid improvement in the patient’s condition. Once infection markers cleared, the patient was immediately placed on the transplant waiting list, and an organ was secured without delay. The patient has since recovered fully, with both heart and the new lung functioning normally more than two years post-operation.
This successful deployment, the first recorded use of this specific artificial lung apparatus in a human, moves the concept of total respiratory replacement from theoretical possibility to clinical reality. It offers a critical lifeline in scenarios where native lung function is lost due to acute injury or overwhelming infection, potentially expanding the window for successful donor matching.
The development underscores ongoing global efforts in bioengineering to create robust, temporary substitutes for failing vital organs. The ability to sustain a patient indefinitely, or at least for the necessary bridging period, represents a major technical hurdle overcome in transplant medicine, as reported by the Northwestern team on January 29.